Services
- Hepatology
- Cirrhosis
- Hepatitis
- Liver Transplant
- HCC
Liver Transplant
Liver transplant is a surgical procedure performed to replace a diseased or damaged liver with a healthy liver from a donor. It is typically considered for individuals with end-stage liver disease or acute liver failure that cannot be managed effectively with medical treatments or other interventions. End-stage liver disease can result from various causes, including chronic viral hepatitis (such as hepatitis B or C), alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), autoimmune liver diseases, genetic disorders, or certain cancers affecting the liver.
The liver transplant process involves several steps: first, the patient undergoes extensive medical evaluation to assess their overall health and suitability for transplantation. Once deemed eligible, they are placed on a waiting list for a suitable donor liver, which can come from a deceased donor (deceased donor liver transplant) or a living donor (living donor liver transplant). Deceased donor organs are allocated based on factors such as blood type, body size, and medical urgency.
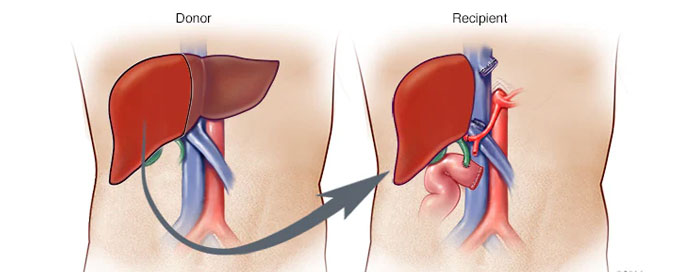
During the transplant surgery, the diseased liver is removed, and the healthy donor liver is implanted and connected to the patient's blood vessels and bile ducts. The procedure can take several hours, and intensive post-operative care is required to monitor for complications such as rejection of the new liver, infections, or surgical complications.
Liver transplant offers the potential for improved quality of life and long-term survival for individuals with end-stage liver disease. After transplantation, lifelong immunosuppressive medications are necessary to prevent the body from rejecting the donor liver. Regular medical follow-up and monitoring are essential to assess liver function, manage medications, and address any potential complications.