Services
Esophageal, Gastric, Duodenal Stenting
Esophageal, gastric, and duodenal stenting are medical procedures used to relieve obstructions in the upper gastrointestinal (GI) tract, which can be caused by various conditions such as tumors, strictures, or benign blockages. The procedure involves the placement of a stent, a flexible, tubular device that helps keep the passage open, allowing food and liquids to pass through more easily.
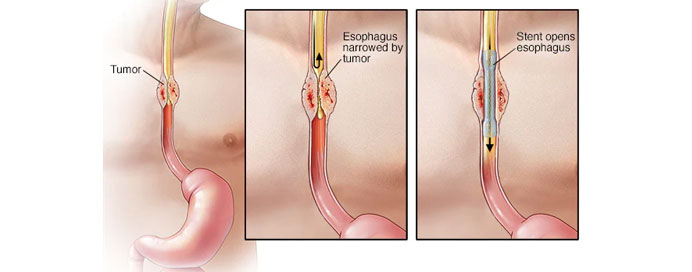
Esophageal Stenting
Esophageal stenting is commonly used to treat obstructions caused by esophageal cancer or strictures from other diseases. An endoscope is used to guide the stent into place within the esophagus. The stent expands once deployed, providing a clear passage for swallowing. This procedure significantly improves the patient's ability to eat and drink, enhancing their quality of life.
Gastric Stenting
Gastric stenting addresses blockages in the stomach, often resulting from tumors or benign pyloric stenosis. The stent is placed endoscopically, ensuring that the passage between the stomach and the small intestine remains open. This procedure alleviates symptoms such as nausea, vomiting, and abdominal pain caused by gastric outlet obstruction.
Duodenal Stenting
Duodenal stenting is used for obstructions in the duodenum, the first part of the small intestine. These obstructions are typically due to malignancies like pancreatic or duodenal cancer. Endoscopic placement of the stent helps restore the passage of food and digestive juices, relieving symptoms and improving nutrient intake.
In all three types of stenting, the procedure is minimally invasive and performed under sedation. The stents are usually made of metal or plastic and are designed to be flexible and self-expanding. The benefits of stenting include immediate relief from obstruction symptoms, reduced need for more invasive surgical interventions, and relatively quick recovery times.