Services
- Hepatology
- Cirrhosis
- Hepatitis
- Liver Transplant
- HCC
HCC
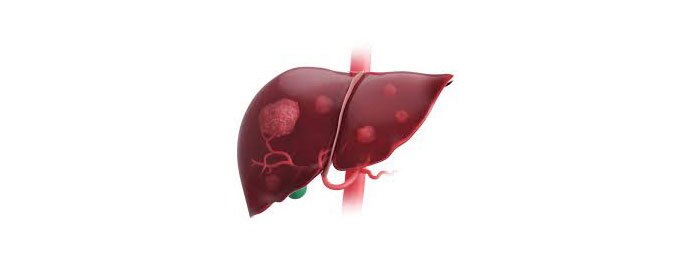
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, accounting for the majority of cases worldwide. It typically arises in the setting of chronic liver disease and cirrhosis, with risk factors including chronic viral hepatitis (such as hepatitis B and C), alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), and certain genetic disorders. HCC often presents at an advanced stage and is associated with poor prognosis, making early detection and treatment crucial for improving outcomes. Symptoms of HCC may include abdominal pain, weight loss, jaundice, and a palpable mass in the abdomen. Diagnosis is typically confirmed through imaging studies such as ultrasound, CT scan, or MRI, and may be supplemented by biopsy to evaluate the tumor's characteristics and guide treatment decisions. Management of HCC depends on factors such as the stage of the disease, the patient's overall health, and tumor characteristics. Treatment options may include surgical resection, liver transplantation, locoregional therapies such as radiofrequency ablation or transarterial chemoembolization (TACE), and systemic therapies such as targeted agents or immunotherapy. The choice of treatment is individualized based on a multidisciplinary approach, aiming to achieve tumor control, prolong survival, and preserve liver function. Prevention strategies such as hepatitis B vaccination, screening and treatment of chronic liver disease, and lifestyle modifications to reduce alcohol consumption and obesity play a crucial role in reducing the risk of HCC development. Overall, HCC represents a significant public health concern, and efforts to improve early detection, optimize treatment strategies, and address underlying risk factors are essential for reducing its impact on global health.